Microsoft is helping epilepsy patients predict when they will have a seizure
People with epilepsy could soon be able to predict when they will have a seizure under a “pioneering” project that uses Microsoft products to monitor health.
MyCareCentric Epilepsy, a program run by a private/public consortium, will see patients wear a Microsoft Band to record data such as sleep patterns, exercise, heart rate and temperature.
This information will be used alongside a log of when seizures occur and a patient’s medical records to build up the individual’s condition. Over time, Microsoft Azure – the company’s cloud computing service – could potentially “learn” when someone is about to have a seizure and warn them before it happens.
An estimated 600,000 people in the UK – almost one in 100 – are believed to suffer from epilepsy, and around 87 new diagnoses are made every day. The neurological condition costs the National Health Service £2bn annually to treat, with epilepsy leading to 3% of Accident and Emergency visits and a total of 1.3 million days in hospital a year.
It is hoped MyCareCentric Epilepsy – which has been developed by Poole Hospital NHS Foundation Trust, the University of Kent, Shearwater Systems and Graphnet Health – will lead to better care and reduce the cost to the public sector.
Dr Christos Efstratiou, head of the University of Kent research team, said: “Wearable technologies have massive potential to transform the way healthcare is delivered. Coupled with advanced activity tracking algorithms, we are able to now monitor patients on a day to day basis. This will allow clinicians to better assess the effectiveness of medications, and enhance personalised care.”
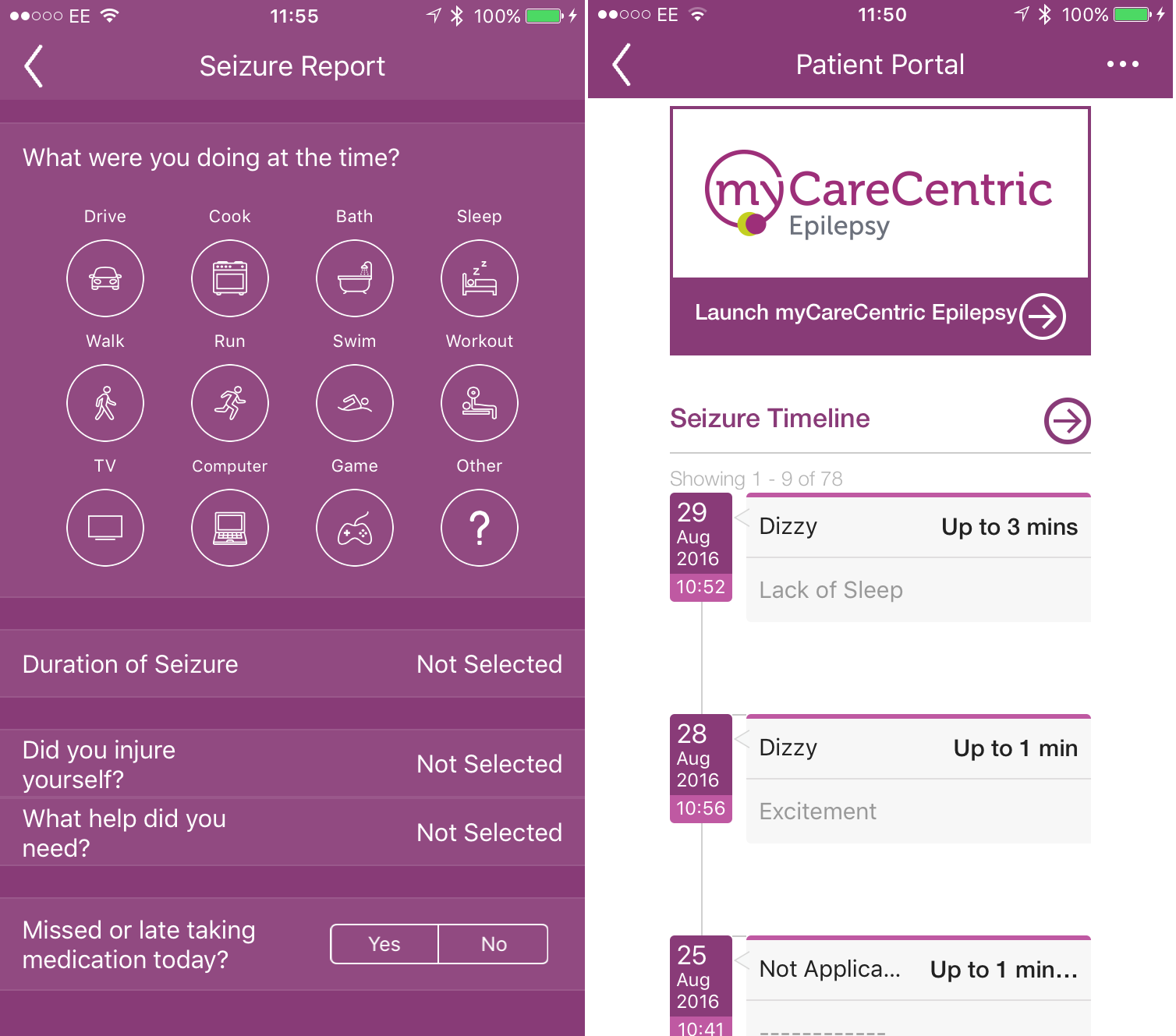
The MyCareCentric Epilepsy app
Suzy Foster, Microsoft’s health and life sciences director, said she was hopeful that the consortium and its technology could help people with other conditions.
“This pioneering project has the potential to redefine the delivery of epilepsy care,” she said. “It is so exciting to see how the latest developments in technology are being used to improve individuals’ treatment and quality of life. We are looking forward to the next phase, where our partners use their technology and market presence to roll out applications for other conditions and disease groups.”
MyCareCentric Epilepsy uses wearables, machine learning, clinical records and data analysis to share information with patients and medical professionals in real-time. Clinicians can access the findings, which could potentially also include video and audio recordings if a patient gives their consent, 24 hours a day online or via a smartphone app.
It is hoped the system will be developed further to alert medial staff, family and friends when a patient has a seizure, and allow professionals to use the app to provide advice to the person affected.
Patient Sean Hamilton signed up for the service as soon as he heard about it. “The one key thing for me is about being able to have a safety net and a support system so I can actually regain my independence,” he said. “What tends to happen now, particularly if I am out on my own, is that I end up back in an ambulance or in A&E. I hope to get better control of my seizures and ideally to get the life back that I used to have.”
MyCareCentric Epilepsy was co-funded by Innovate UK and is currently being piloted by Poole Hospital and the Dorset Epilepsy Service.
Dr Rupert Page, consultant neurologist and clinical lead for the Dorset Epilepsy Service, said he could now focus resources “on those patients who need support, and at their time of need”.
“The novel visualization tools enable us to see critical details at a glance, releasing more time to care”, he added. “And by using wearables, monitoring and notification technology – combined with secure communication to clinical systems – we are providing patients with an electronically-enabled safety net.
“This level of direct engagement helps clinicians monitor and understand the nature of someone’s epilepsy and seizures and respond immediately with alterations to drugs, for example. This has significant quality of life benefits for the patient, and cost benefits to the health service by reducing outpatient and emergency department visits, preventing hospital admissions and cutting medication bills.”