Doctors are using technology to help patients with a serious lung disease get treatment in their homes
Medical experts at one of the largest health boards in Europe are using cutting-edge technology to remotely monitor and treat people with a life-threatening lung condition in their own home.
NHS Greater Glasgow and Clyde believes the trial, which has never been attempted before, will improve care for people with Chronic Obstructive Pulmonary Disease (COPD), result in fewer hospital admissions and save the health service money.
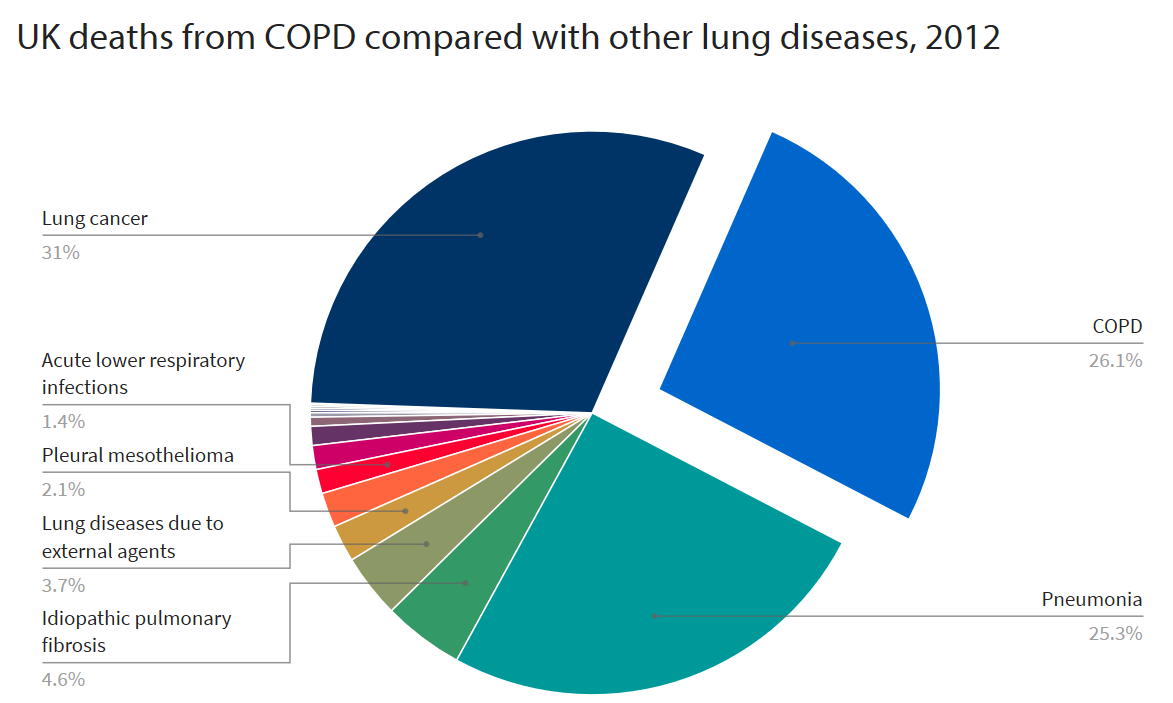
COPD occurs when the lungs become inflamed, damaged and narrowed, and usually affects middle-aged and older people who have smoked or have been exposed to air pollution. Without treatment the symptoms, which include breathlessness, chest infections and a persistent cough, usually get worse. The condition affects 1.2 million people in the UK and is the second most common cause of emergency hospital admissions.
Two NHS consultants in Scotland are now trying to change that by using wearable devices and Microsoft’s Azure cloud platform to remotely monitor COPD patients’ breathing machines in their homes and vary their treatment accordingly.
“We see around 10 COPD patients a day in the emergency department,” said David Lowe, an Emergency Consultant at NHS Greater Glasgow & Clyde. “Avoiding hospital admission is a priority for patients with COPD and has a significant impact on the health service, which is struggling to cope with increased demand. It has an impact on the wellbeing of the patient and costs an average of £6,000 per admission. We could have delivered the same key interventions using antibiotics and steroids to the patient in their home days earlier if we had sight of their decline.”
Chris Carlin, a Consultant Respiratory Physician, added: “It’s about delivering treatment earlier by using data. If we can empower patients to self-manage their condition, we can significantly reduce hospital admissions. That self-management might be helping them with their breathing, escalating their existing treatment, recommending new treatment or reaching out to the community respiratory team.
“The information is already there, so this trial is about making sure it’s integrated and surfaced to clinical teams and the patient.”
By teaming up with KenSci, a company specialising in machine learning that uses Azure to securely store data, and Storm ID, a Microsoft partner that specialises in developing new digitally enabled care models, medics can see patient-reported information and physiology data produced by a patients’ wearable device and their breathing machine, which blows air through a mask at a varying intensity to increase the capacity of the person’s breathing. The patients and clinical team can communicate by messaging through the cloud-based platform, while the consultants can also change the ventilation remotely via an online portal.
“Patients can be empowered to self-manage their condition, with rescue packs of treatment,” Lowe said. “Those can be delivered in the community; but it’s about appropriate treatment, so we are not starting people on steroids and antibiotics for no reason. By using data, we can say to patients: ‘This is when you need to take them to prevent you going to hospital,’ rather than telling people to take it because they might just feel a bit worse.”
The trial will include 400 COPD patients, with the aim of reducing hospital admissions by one a year. If successful, it could be rolled out more widely and used to help people manage other conditions, such as frailty or diabetes.
The health sector is increasingly using cloud technology to improve how it delivers care to patients and reduce costs. In November, NHSScotland signed a “landmark” deal with Microsoft to merge more than 100 separate computer systems and give its 161,000 staff access to Office 365 so they can spend more time focusing on patients. GPs, consultants and support workers will now be able to communicate on one digital platform, allowing them to share patient information more easily and reduce waiting times.